Addressing the opioid epidemic in acute care
Opioid Use Disorder (OUD) often emerges from legally prescribed medications, such as pain medications initiated during an inpatient hospital stay, which can then escalate if factors such as pain management and opioid prescribing are not thoughtful. Managing opioid use in the acute care setting requires a multifaceted Opioid Stewardship Program (OSP). The push for Opioid Stewardship in hospitals is driven by ensuring safe care through preventing adverse drug events and improving the safe and effective use while also adequately controlling pain. In 2018, the Joint Commission targeted these concerns in their release of the Pain Assessment and Management Standards, which are categorized into four chapters:
- Leadership (LD)
- Medical Staff (MS
- Provisions of Care, Treatment and Services (PC)
- Performance Improvement (PI)
Drug overdoses drive the need for opioid stewardship programs
Drug overdose deaths have skyrocketed during the COVID-19 pandemic, in part due to healthcare accessibility and resources being especially limited. According to provisional CDC data released in November 2021, the 12 month-ending number of drug overdose deaths in April 2021 was nearly 100,000, the highest number ever recorded. Several factors contributing to this steep increase in drug overdose include fear surrounding the uncertainty with the COVID-19 pandemic, psychosocial stressors related to increasing unemployment, risk of eviction, and temporary loss of treatment programs such as syringe exchange and naloxone administration.
It is now more imperative than ever to build a robust Opioid Stewardship Program. Nevertheless, executing a plan to implement a program at your own facility is easier said than done. According to a study published in 2018 by Ardeljan et al. only 23% of United States acute care hospitals have adopted an Opioid Stewardship Program.
Goals of opioid stewardship programs
Best practices surrounding Opioid Stewardship vary and depend on many factors in a hospital, such as size, acuity level, specialties, geographic location, etc. However, the most common shared goals include:
- Reduce opioid overuse, misuse, and abuse
- Prevent addiction and sequalae (overdose)
- Improve pain management outcomes while reducing risks (e.g., ADE)
- Increase awareness and treatment of OUD
- Create partnerships between the patient, providers, and the community
- Improve the patient experience
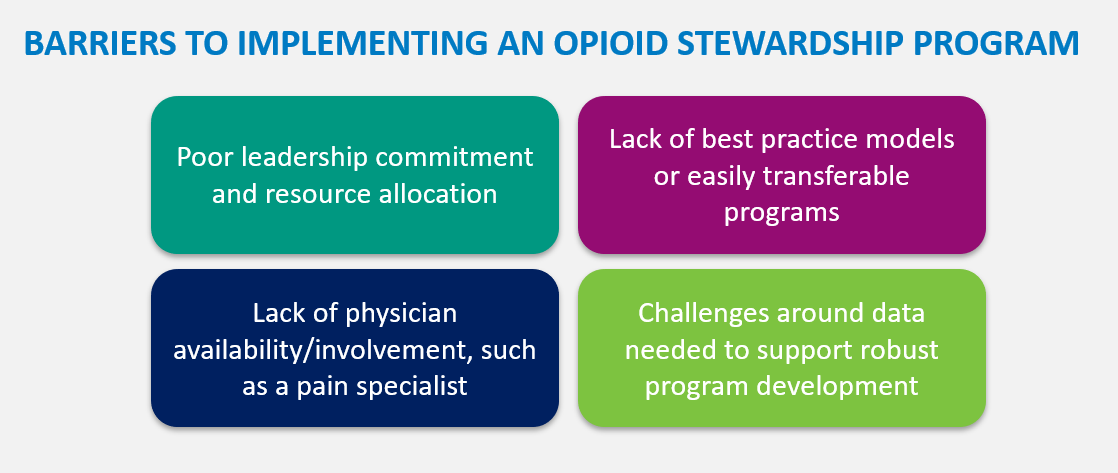
Four barriers to implementing an opioid stewardship program
With these best practices in mind, there are four main barriers to implementing an Opioid Stewardship Program at a hospital or health system.
1. Poor leadership commitment and resource allocation
The foundational groundwork to a strong OSP involves senior leadership that is willing to devote both financial and physical resources. Without this cornerstone, the OSP can be expected to fragment from the start.
2. Lack of best practice models or easily transferrable programs
Trying to standardize and implement an OSP enterprise-wide is one of the biggest challenges faced by pharmacy leadership. It is essential to ensure an organizational or system-level approach. Optimizing the usage of a data-driven tool could alleviate this strain by reducing the burden of physical work on pharmacy staff.
3. Lack of physician availability or involvement
Examples a pain specialist - Interprofessional engagement is essential in the early stages of OSP development, as establishing trust between departments can further strengthen the initiative and lead to widespread adoption.
4. Challenges around the data necessary to support robust program development
This is by far the most complicated barrier to overcome due to factors such as volume or how the data is structured. Not only must the OSP ensure data integrity within its initiatives, the OSP leadership team must know how to utilize and interpret the data to track progress and improve outcomes.
Normalizing opioid use data – the power of Sentri7® Pharmacy’s MME calculation
A data-driven Opioid Stewardship Program utilizing tools such as Sentri7® can promote best practices and overcome several barriers, such as those listed above. Sentri7 provides AI-powered tools that are crucial to improving opioid use and patient safety through evidence-based rules and analytics. During a pilot study involving an Integrated Delivery Network (IDN), novel opportunities in measuring and monitoring opioid use were identified MME is a strategy to normalize doses of opioids with variable potencies, which improves transparency into opioid use. The higher the MME, the greater the risk for a serious ADE.
Normalizing opioid use data is valuable, but it also tremendously difficult in the acute care setting due to many factors such as opioid naming and variation, potency differences, multiple routes of use, poor documentation, combination products, and exclusion of certain uses. Sentri7's Opioid Stewardship was validated during the pilot study with the IDN. Anticipating the expected MME allowed the pharmacy team in the pilot program to understand opioid use patterns, evaluate inappropriate use, launch improvement efforts, and support continuous improvement in their clinical initiatives.
The pilot study also identified opportunities to increase the IDN’s use of multi-modal therapies for pain management, which can prevent over-sedation events and reduce the risk of other side effects associated with opioids. Moreover, the pilot study revealed the value of real-time interventions on MME > 90 per day, identification of opioids co-administered with benzodiazepines, and lack of bowel regimen for patients receiving opioids. This versatile approach to rule-based, inpatient-focused, opioid stewardship provides real-time surveillance coupled with evidence-based, clear opportunities for intervention.
Tackling opioid stewardship with teams and technology
As the opioid crisis continues to worsen in the United States, hospitals are driven to support tackling this epidemic and pharmacy teams are imperative in these efforts. By identifying goals for an Opioid Stewardship Program, recognizing, and overcoming barriers to entry, implementing best practices, and leveraging tools to support a data-driven program, hospitals can start to see success in operationalizing pain management strategies.
Learn how pharmacy teams can take a leadership role in opioid stewardship programs in our free guide.